Induction Of Labour – A Critical View
If you are offered induction of labour by your healthcare provider, it is important to find out why this has been suggested considering your personal circumstances, and to make a decision that is right for you.
What is induction of labour?
Labour induction is a procedure that is performed when a pregnancy is at or beyond its due date, or when there are medical reasons to expedite the delivery. The goal of induction is to start labour artificially so that the baby can be delivered safely. While induction can be a life-saving intervention, it is important to recognize that over-medicalisation as a standard can have a negative impact on your health and wellbeing. You should be fully informed about the risks and benefits of induction, and the fact that it is not always a quick process. Induction can sometimes take several days as your body may not be ready to undertake, and your hospital stay may be prolonged compared to a spontaneous labour. Before and during induction, vaginal examinations are necessary to evaluate the cervix, determine the optimal method of induction, and monitor progress. Furthermore, the options for the place of birth may be restricted as some interventions, such as oxytocin infusion, continuous fetal heart rate monitoring, and epidurals, will not be available in home birth or midwife-led birth units. It is important to note that induction of labour is a medical process that may affect your birth options and your overall experience of birth, and you may accept or decline this intervention at any point.
What happens during an induction?
When your labour is induced, quite often there may be a need for epidural due to the increased intensity of your contractions. Therefore, there may be a requirement for an assisted vaginal birth, which involves the use of forceps or ventouse, increasing the risk of obstetric anal sphincter injury, including third- or fourth-degree perineal tears. Pharmacological methods of induction may result in hyperstimulation, where the uterus contracts too frequently or for too long, leading to changes in fetal heart rate and potentially compromising the baby.
You may also be required to have continuous monitoring of your baby via cardiography (CTG).
Methods of induction:
There are various methods of induction:
-
Balloon inserted into the cervix using a sterile tool by an experienced practitioner or doctor.

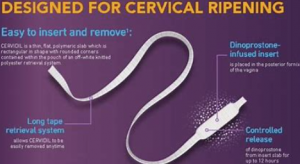
- Cervical ripening using a pessary or gel into the cervix. This sits just behind the cervix slowly releasing prostaglandins to soften the cervix
- Artificial rupture of membranes
-
Administration of synthetic oxytocin through a drip.

This method requires access to your vein via a cannula to administer the medication.
These methods vary from trust to trust so you may need to contact your healthcare provider to obtain information on their local policy and guideline for induction.
Reasons for induction:
In the UK, induction of labour (IOL) is performed on approximately 20% of pregnant women. The primary reasons for IOL are discussed below.
Postdates:
The most common reason for IOL is being “overdue.” The National Institute of Clinical Excellence (NICE) provides healthcare guidelines in the UK, which suggest that IOL should be offered between 41 and 42 weeks of pregnancy to ensure the baby is born by 42 weeks. Evidence supporting this guideline shows that the rate of stillbirth is lower for women who have induction before 42 weeks (0.4 per thousand) than those who go beyond 42 weeks (3 per thousand). There is no difference in the rate of instrumental births or caesarean between the two groups. However, the decision to go beyond 42 weeks or undergo induction is a personal one that individuals should make based on their own circumstances and risk tolerance. Many healthcare professionals rationalise induction for this reason due to the fact they believe that the placenta may begin to fail past a certain point in pregnancy. Although there is no evidence to support this claim, as many babies are born past 42 weeks with healthy babies and placentas. Why would the organ that has been supporting your baby throughout suddenly decide to not function as before? Many believe that the placenta adapts as pregnancy develops to support the baby as it needs to.
Here is some useful information regarding induction at term and statistics of still birth rate according to gestation. It shows that women who decide to await events and give birth beyond 42 weeks are at a decreased risk of still birth.
https://www.aims.org.uk/journal/item/induction-at-term
https://evidencebasedbirth.com/studies-that-calculate-risk-of-stillbirth-by-gestational-age/
Maternal Age:
Women aged 35 or older are offered IOL in the UK due to an increased risk of stillbirth if they go beyond 40 weeks of pregnancy. However, if a woman has had a previous baby, the risk of stillbirth is lower.
If you are over the age of 35 you are at a small increased risk of still birth but when you look at various studies, you will find that the risk goes from 0.4 to 0.6% for women over the age of 35. The risk increases to 0.8% if you are over the age of 40. Doctors may tell you that your risk doubles, but this is relative risk. The absolute risk is very small, and many studies do not factor in morbidity in the women or lifestyle choices. Many of these studies took into account women who birthed more than 50 years ago. Things are very different now and the stillbirth rate has decreased significantly in recent years. Take a look at evidence-based birth which shows the statistics from many studies in the Uk and worldwide.
https://evidencebasedbirth.com/advanced-maternal-age/
Suspected large baby:
Many women go for a scan at 36 weeks and are told that their baby is large and are recommended induction for this reason. However, scans have a large margin of error up to 20% and therefore should not be advised to induce their labour for this reason alone. Women have been known to birth babies that are considered large (over 10lbs) with no complications at all and even have had no tearing of their perineum. This can be achieved by birthing upright and not on your back as the pressure is decreased in your perinium in these positions, as well as ‘coached pushing’. If you follow your body and gently breathe your baby down the birth canal this can significantly decrease your risk of tearing. The concern with a big baby is a complication known as shoulder dystocia whereby the shoulder becomes impacted against the pelvic bone and is difficult to be born. Many babies under the birth weight of 8lbs can also experience a shoulder dystocia, so weight of the baby should not be considered. If you have diabetes for instance, this may present a problem as your baby is likely to be on the larger side with broader shoulders and may have difficulty navigating the pelvis.
Suspected small baby or growth restriction:
It is very important to understand that they are two different things.
A small baby may be due to the fact that you grow babies of that size and not necessarily be a problem at all. However, if you have been told that your baby is small due to growth restriction then it may be that your baby is not obtaining enough nutrients and oxygen from the placenta and induction may be the best option for you under these circumstances. Your sonographer will check for blood flow to the baby and will inform you if this has been compromised in some way.
Medical Reasons:
IOL may be offered for medical reasons, including diabetes, obstetric cholestasis, high blood pressure, pre-eclampsia. When considering IOL for medical reasons, reviewing the relevant research and data can help individuals make an informed decision.
Pros and Cons of Induction:
When making a decision about IOL, individuals should weigh the pros and cons based on their individual circumstances. The pros include feeling that IOL is the safest choice for the baby, being able to start the process as an outpatient or on the midwifery-led unit and feeling ready to give birth. The cons include the possibility of a longer hospital stay, more intense and less manageable labour, the need for a doctor-led unit if a syntocinon drip is required, the potential for IOL to fail resulting in a caesarean and feeling unprepared to give birth.
Induction is not a decision that should be taken lightly. It is important for you to have a clear understanding of the reasons why induction is being recommended, the risks and benefits, and the alternatives. For example, if induction is being recommended because the pregnancy has gone beyond the due date, women should be aware that waiting for labour to start spontaneously is also an option. Similarly, if induction is being recommended due to a medical concern, women should understand the nature of the concern and the options for managing it.
One of the risks associated with induction is that it can lead to a longer labour. This is because the body may not be fully prepared for labour and may need more time to respond to the artificial stimulation. This can increase the likelihood of interventions such as assisted delivery and may also increase the risk of complications such as infection. Another risk is that induction can lead to a more painful labour, as the contractions may be stronger and more frequent than they would be in a natural labour.
Over-medicalisation of childbirth is a concern in many countries, as it can lead to unnecessary interventions. You have the right to make informed choices about your care and should be given the information and support to make decisions that are right for you. This means that healthcare providers should be transparent about the reasons for recommending induction and should provide clear information about the risks and benefits. Women should also be encouraged to ask questions and to seek additional information if they are uncertain about any aspect of their care.
In conclusion, induction of labour is an important intervention that can help to ensure the safe delivery of a baby. However, it is not a decision that should be taken lightly. Women should be fully informed about the reasons for induction, the risks and benefits, and the alternatives. They should also be aware that induction is not always a quick process, and that it can lead to a longer and more painful labour. Over-medicalisation of childbirth is a concern, and women should be given the information and support they need to make informed choices about their care.
I offer worldwide remote support and information during pregnancy and birth. visit my home page to find out more about me:
https://loucinabirthkeeping.co.uk/home/
However, if you would like more information about a Birth keeper near you for in person support, you can contact:
https://www.whenpushcomestoshove.co.uk/your-pregnancy
They have over 100 Birth keepers and doulas on their directory in several countries world wide.






